Treatment of Periodontal Disease
Periodontitis is a serious infection of the tissues that support the teeth, referred to collectively by your dentist as the “periodontium” (“peri-” means around, and “-odont-” means tooth). The periodontium includes the gums, the ligaments that hold your teeth in place, and the jawbone.
If periodontitis is left untreated, it can lead to irreversible destruction of these tissues. The patient can experience bleeding and receding gums, painful abscesses, and tooth loss.
The good news is, periodontal disease is treatable and preventable, especially in its earlier stages. Our dentists and hygienists are trained to identify periodontal disease, and will help to develop a personalized and ongoing treatment plan of periodontal therapy and maintenance.
What is the Difference Between Gingivitis and Periodontitis?
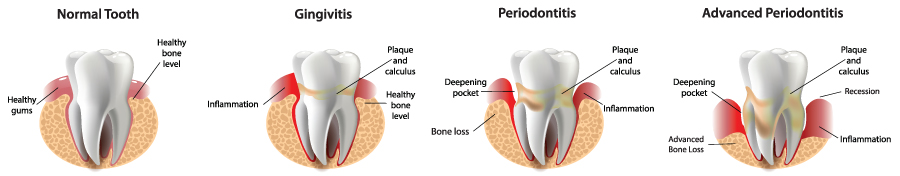
Most people have heard of gingivitis, but what is periodontitis? To put it simply, gingivitis and periodontitis are two different stages of gum disease.
Gum disease works like this: plaque and calculus accumulate on your teeth over time. This buildup on your teeth and under your gums harbors infectious bacteria. The bacteria trigger your immune system to fight off the infection, just like when you have a cold or flu. Those immune cells rush to the areas around your teeth, causing the gums to swell and bleed. The harder our immune system has to work to fight the bacteria in our gums, the more likely it is that the tissues around the teeth will become damaged.
The first sign of damage to the tissues is swelling and bleeding of the gums. This is what we call gingivitis, an earlier stage of gum disease. When you have gingivitis, your teeth have not yet lost their attachment to the surrounding bone. If we don’t get gingivitis under control with good oral hygiene and regular professional dental cleanings, the inflammation of the gums continues to progress.
The infection spreads to the surrounding tissues, and our immune system starts to irreversibly destroy the bone around the teeth. Once you’ve reached this stage of gum disease, you are diagnosed with periodontitis. The teeth begin to lose their attachment to the jawbone. You may experience swollen and bleeding tissues, receding gums, discomfort when brushing or flossing, bad breath, or painful abscesses around the teeth.
If periodontitis is left unchecked, the teeth eventually become so loose or infected that they have to be extracted. There is also a growing body of evidence that periodontal disease may be linked to systemic diseases such as diabetes, heart disease, and even some cancers.
We categorize periodontitis as early, moderate, or advanced/severe, depending on how much bone has been lost already. Periodontal therapy and ongoing maintenance are critical for reducing inflammation, stabilizing your teeth’s supporting tissues, and preventing further jawbone loss.
What Causes Periodontal Disease?
The bacteria found in dental plaque is the main cause of periodontal disease. Good oral hygiene, including daily brushing and flossing and routine professional dental cleanings can help to keep plaque and calculus levels under control.
Several other factors can contribute to gum disease as well, including some underlying medical conditions, medications, or bad habits. These factors may increase your risk of developing a gum infection, and can make an existing infection worse. A few are described below.
Genes – Some patients are more genetically prone to gum disease. However, even with a genetic predisposition, gum disease is not inevitable. If you know you have a family history of gum disease, it is simply that much more important to adopt excellent oral hygiene practices and see your dentist for routine checkups and professional dental cleanings. Your dentist and hygienist can work with you to develop a plan to mitigate your risks.
Fluctuating Hormones – The risk of gum disease can fluctuate as the body’s hormones go up and down. Patients going through puberty, pregnancy, or even menopause may temporarily be at higher risk for gingival diseases. Your dentist and hygienist can help you to maintain your gingival health and minimize the impact of hormone fluctuation on oral tissues.
Diabetes – Patients with diabetes are more likely to develop periodontal disease than patients without diabetes, and diabetes can make existing periodontal disease more difficult to control. Diabetic patients with periodontal disease may benefit from a more extensive regimen of periodontal therapy and more frequent recall visits. Your dentist can give you guidance about how to manage your periodontal disease when you have an underlying diagnosis of diabetes.
Smoking and Tobacco Use – This is a big one. Smoking not only puts a patient at higher risk for periodontal disease, but it can also make periodontal disease much more severe. It is often a reason that periodontal disease is resistant to treatment. And, unlike many other factors that increase your risk of periodontal disease, the use or non-use of tobacco is entirely under a patient’s control. There are a lot of great reasons to quit smoking and using tobacco, and your oral health is one of them. We encourage our patients to quit smoking to help bring their periodontal disease under control, and we can help point you toward resources when you’re ready to quit.
How is Periodontitis Treated?
Periodontitis is treated with a personalized and ongoing therapy program designed to reduce inflammation, restore the gums to a firm and healthy state, and stabilize the teeth and gums so that further jawbone attachment loss can be prevented.
Periodontal therapy is often divided into two categories: Active Therapy, and Maintenance.
Active Therapy – The most common active treatment of periodontal disease is periodontal scaling and root planing, sometimes referred to as a “deep” cleaning. Scaling and root planing is a specialized kind of dental cleaning that removes plaque, calculus, and diseased cementum from the sides of the tooth roots. It is most often performed by a dental hygienist, and may include topical or local anesthetic. If multiple areas of the mouth are involved, treatment is often spread out over a few appointments for best results and patient comfort.
In more severe or resistant cases, your dentist may consider special antibiotics or a referral to a dental specialist called a periodontist. A periodontist can evaluate you for more specialized treatments, like tissue grafting or other surgical procedures.
Maintenance – Your dentist and hygienist will develop an ongoing plan to keep the dentition healthy and stable after we’ve seen the benefits of active therapy. This is how we protect the good work we’ve accomplished together and stay on top of any future signs of disease progression.
Maintenance typically involves a personalized home care plan focused on excellent oral hygiene, as well as specialized follow up appointments called periodontal maintenance visits. When a patient has lost bone around the teeth, “regular” dental cleanings may no longer be enough to keep your dentition healthy.
Periodontal maintenance visits are designed for patients with a history of periodontal disease, and include the removal of bacteria above and below the gumline, scaling and polishing of the teeth as needed, ongoing periodontal evaluation, and a regular review of the patient’s ability to control plaque and bacteria. If new or recurring periodontal disease is discovered at a periodontal maintenance visit, additional active therapy may be recommended.
Periodontal maintenance visits are important for protecting the continued health of your gums and preventing further loss of jaw bone around the teeth. Patients with a history of gum disease are at high risk for continued disease progression, so periodontal maintenance visits are often recommended more frequently, every three or four months.
My Teeth Feel Fine. Why Do I Need Treatment For My Gums?
Many patients know that swollen and bleeding gums mean that the tissues around the teeth are unhealthy. Some patients start to notice the roots of their teeth showing as the gums start to recede back or the discomfort and sensitivity they feel when brushing. Maybe a loved one has noticed bad breath.
However, many patients do not notice the signs or symptoms of gum disease until much later in the disease process, like when the teeth start to feel loose. Unfortunately, it is sometimes too late to achieve an ideal result when the disease has progressed this far, and we have to start planning for more extensive treatments, like tooth extraction, implants, and dentures.
Like many other areas of dentistry and healthcare, it is best to address problems in their earlier stages, when they are more manageable. If you have questions for your dentist or hygienist about what periodontal disease is or how you may have been diagnosed with this condition, please ask us! We’re here to help you understand your oral health and empower you to make the right decisions to preserve the health of your smile.
I’ve Been Diagnosed with Periodontitis. Why Do I Need a Special Kind of Cleaning?
Many people don’t know that there are different kinds of dental cleanings. The type of cleaning you need depends on the condition of your teeth and gums. Common types of cleanings include prophylaxis, periodontal scaling and root planing, and periodontal maintenance. Learn more about each one below.
Prophylaxis – A prophylaxis (a “regular” cleaning) is recommended in combination with excellent home care to prevent dental problems. A prophylaxis is performed in a healthy mouth that is free from gum disease or bone loss.
Periodontal Scaling and Root Planing – If active gum disease and progressive bone loss is identified during your exam, your dentist may recommend periodontal scaling and root planing, sometimes referred to as a “deep” cleaning. This is a non-surgical procedure that removes the plaque, calculus, and diseased cementum from the surfaces of the affected tooth roots.
This is a procedure performed by your dental hygienist, often with topical numbing agents or local anesthesia. If multiple areas of the mouth require scaling and root planing, treatments are often spread out over a few appointments for best results and patient comfort.
Signs that you may need this type of cleaning include swollen red gums that bleed when you brush or floss, deep pockets in the gums around your teeth, or bad breath.
Periodontal scaling and root planing is not a “once and done” kind of procedure, and a personalized and ongoing maintenance plan is a critical part of your therapy. We work closely with patients who have been diagnosed with periodontal disease to develop individualized home care plans and professional care follow up, typically including periodontal maintenance visits.
Periodontal Maintenance – Once a procedure like periodontal scaling and root planing has been completed, routine prophylaxis cleanings may no longer be enough to keep your dentition healthy. Often, your dentist may recommend a specialized follow up cleaning called periodontal maintenance.
Periodontal maintenance visits are designed for patients with a history of periodontal disease, and include the removal of bacteria above and below the gumline, scaling and polishing of the teeth as needed, ongoing periodontal evaluation, and a regular review of the patient’s ability to control plaque and bacteria. If new or recurring periodontal disease is discovered at a periodontal maintenance visit, additional active therapy may be recommended.
Periodontal maintenance visits are important for protecting the continued health of your gums, and preventing further loss of jaw bone around the teeth. Patients with a history of gum disease are at high risk for continued disease progression, so periodontal maintenance visits are often recommended more frequently, every three or four months.
 Cameo Dental – Family Dentistry in Rosemount Minnesota
Cameo Dental – Family Dentistry in Rosemount Minnesota